What does the GP Patient Survey tell us about people with long term mental health conditions?

Mental health has been a priority area for policymakers for many years. There has been a particular emphasis on mental health recently, with the government pledging to put mental health on a par with physical health.
We know from our research for the Department of Health (DH) that concern among the general public about mental health is rising; the proportion mentioning it as a problem has risen in recent years, particularly among young people. In addition, recent work on interest in science and medical research for the Wellcome Trust found that mental health is of the greatest interest to the public from a range of specific research areas and the proportion expressing this interest has increased significantly from 48% in 2012 to 55% in 2015.
The GP Patient Survey (GPPS) helps us understand a little bit more about the experiences of patients reporting a long-term mental health condition, in relation to general practice.
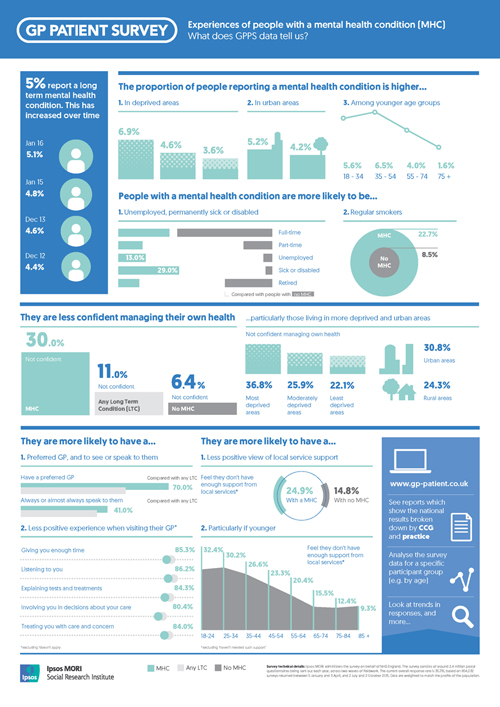
The proportion reporting a long-term mental health condition in GPPS has increased slightly over the past four years (from 4.4% in December 2012 to 5.1% in January this year). We see higher proportions of people reporting a mental health condition in deprived areas and urban areas, as well as among younger age groups. GPPS data also shows that people with mental health conditions are more likely to be unemployed or permanently sick and disabled compared with people without a mental health condition. They are also more likely to be regular smokers.
Almost a third of these patients (30.0%) say they are not confident managing their condition. This is significantly higher than for all people without a mental health condition (6.4%). Furthermore, it is also significantly higher when compared to patients with any long-term condition, including mental health (11.0%). This lack of confidence is particularly prevalent in deprived and urban areas (where we see a higher incidence of people reporting a long-term mental health condition).
In terms of their experience of health services, people reporting a long-term mental health condition are more likely to have a preferred GP at their GP practice (70.0% compared to 49.7% with any long term condition, including mental health). Encouragingly, they are more likely to see this GP all or almost all the time and high proportions say their GP was good at giving them enough time; listening to them; explaining tests and treatments; involving them in decisions and treating them with care and concern. However, they are slightly less positive about these aspects of their last appointment than patients with a long term condition overall.
Of course it’s not just the GP practice where support can be found; however almost a quarter (24.9%) of people with a long-term mental health condition say they do not have enough support from local services or organisations to help manage their condition; a significantly greater proportion than among all people who do not have one (14.8%).
Younger patients are particularly likely to say they do not have enough support from local services; this is true both of people with a long-term mental health condition and people with long term conditions overall (see also Ipsos's infographic on long term conditions). However, younger people with a mental health condition are particularly likely to say they do not have enough support.
We also know that public perception of the care available to people with mental health conditions is poor. Ipsos’s research for the Department of Health (DH) on perceptions of the NHS and social care shows that people are more likely to feel those with mental health conditions are not well cared for than feel they are (39% and 31% respectively), and the proportion feeling they are not well cared for has increased since 2013.
Key
- Mental health condition (MHC): anyone who says they have a long term MHC at Q31 in GPPS
- Any long term condition (LTC): anyone who says they have a LTC at Q30 in GPPS, including MHC
- No MHC: anyone who does not select MHC at Q31 in GPPS
Further analysis
GPPS provides a rich source of information on patient experiences of their GP practice. You can access and analyse the results by going to www.gp-patient.co.uk or email the team.
Technical note
Ipsos administers GPPS on behalf of NHS England. The survey consists of around 2.4 million postal questionnaires being sent out each year, across two waves of fieldwork. The current overall response rate is 35.7%, based on 854,032 surveys returned between 5 January and 3 April 2015, and 2 July and 2 October 2015. Data are weighted to match the profile of the population. Read further technical information about how the survey works.
For more information about the survey, and access to the data see www.gp-patient.co.uk.