The NHS at a crossroads: Measuring how the 10-Year Plan will deliver on patient needs
This is a joint article by National Voices and Ipsos in the UK. It is authored by Jacob Lant (Chief Executive, National Voices) and Molly Dawson (Research Manager, Ipsos).
The landscape of patient experience is changing. Historically, measurements of patient experience have been siloed, focusing on individual clinical/service areas within the NHS, or specific patient groups. However, as the system moves towards greater integration, and with patients reporting a lack of joined-up care, a more holistic approach to understanding patient experience is needed. This Ipsos/ National Voices survey aims to address this, measuring patients’ experiences of NHS services in England against the ‘I’ statements that were used to frame the development of the NHS 10 Year Plan.
Why are we doing this now?
At the heart of the 10 Year Plan the Government is aiming to achieve a triple shift - moving care from hospitals into the community, continuing the move from analogue to digital, and more of a focus on prevention rather than sickness.
The detail on how we go about achieving these three shifts is yet to be seen. However, what is clear is that we need an effective system in place to measure and track any improvements – or indeed unintended consequences. This is where our new survey comes into play. It is structured around series of “I” statements, a methodology championed by National Voices. The statements we tracked against are the four the Government said they want the 10 Year Plan to focus on:
- I can stay healthy and manage my health in a way that works for me.
- I can access the high-quality and effective care I need, when and where I need it.
- My care is centred around my needs and I am listened to.
- I am treated in a fair and inclusive way, irrespective of who I am.
By examining patients’ experiences in relation to these 'I' statements, we can identify areas where the NHS is already doing well, areas for improvement, and most significantly, any disparities in experience that highlight persisting health inequalities.
This survey acts as a baseline for understanding patients’ holistic experiences of NHS services at the start of the Plan. Future measurement using this framework would enable us to assess the impact of the proposed changes outlined in the 10 Year Plan, understanding its impact on integrated care and in a way that places the patient – rather than NHS structures – at the centre.
So what does the research tell us?
Overall findings reveal a largely positive picture in terms of peoples’ experiences of the NHS, echoing findings from other research. People generally report positive experiences once they are in direct contact with healthcare professionals. This suggests that the government may have a challenging task to maintain these positive experiences while navigating the potentially significant changes proposed in the 10 Year Plan.
While overall sentiment is positive – for example over 7 in 10 (73%) of the public feel that the care they received reflected their needs – the strength of that sentiment is underwhelming. Just 43% say their care definitely reflected their needs, showing plenty of room for improvement. This gap highlights the need for a continued focus on ensuring patient needs are consistently and fully met.
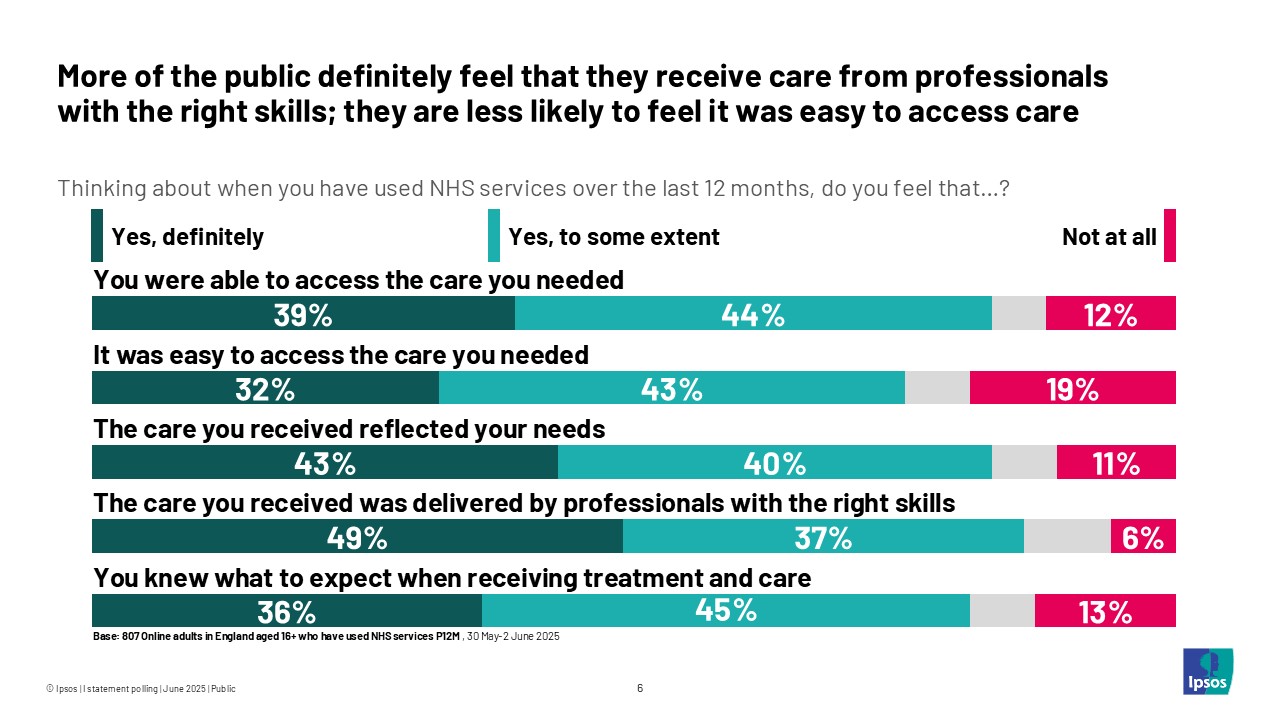
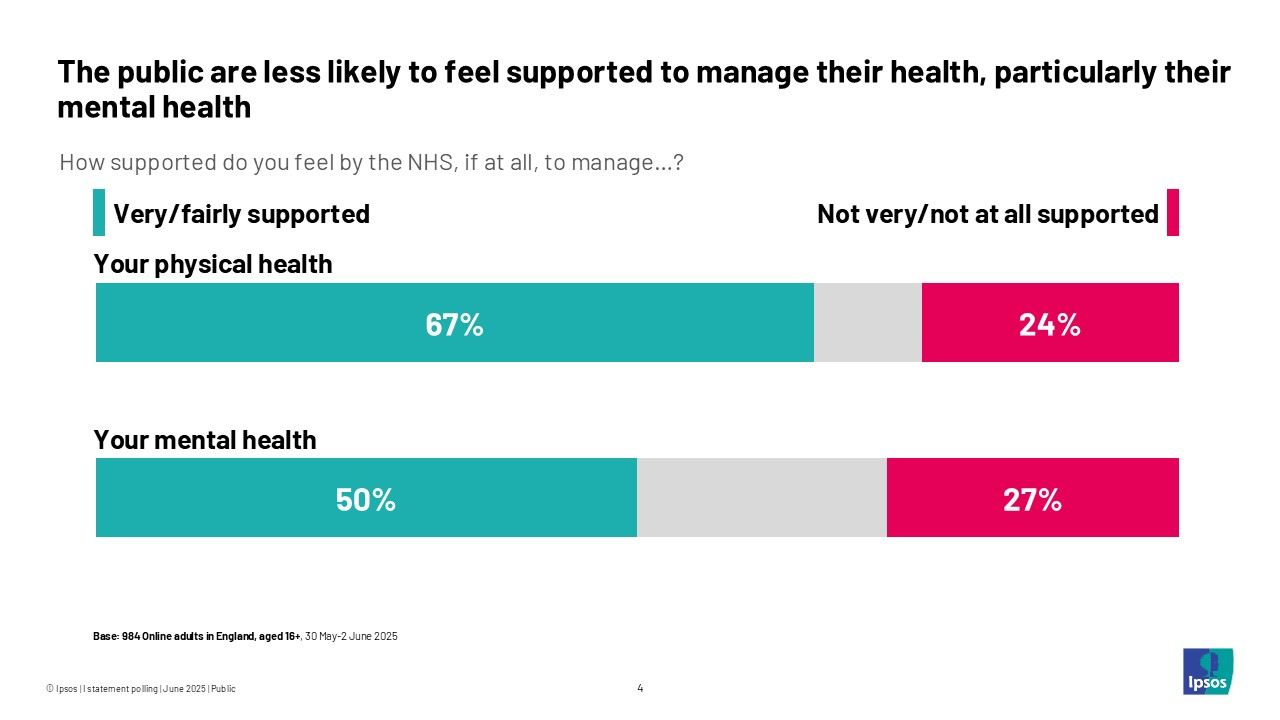
There are several areas where patients report less positive experiences, including access to care, feeling informed while waiting for treatment and feeling supported to manage health (particularly mental health). And just half (50%) say they feel supported to manage their mental health. These identify clear areas that the 10 Year Plan would ideally improve.
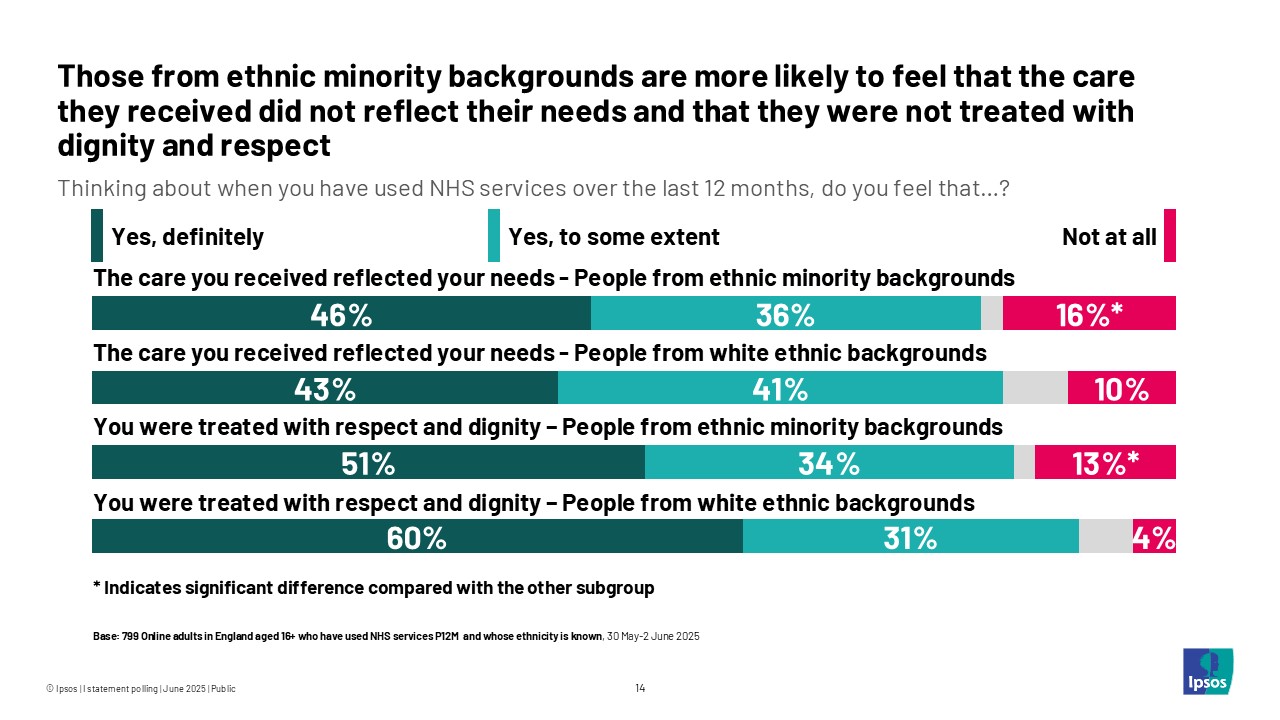
Our research has also revealed some stark health inequalities. For example, people from ethnic minority backgrounds are more likely than those from White ethnic backgrounds to say they were not treated with dignity and respect at all (13% compared with 4%).
People who have multiple long-term health conditions are possibly the most regular users of NHS services. Nearly two in five (37%) of those with more than one long-term health condition say they do not feel supported by the NHS to manage their physical health. This compares with 16% of those with no long-term conditions. The figure rises to 40% when it comes to mental health, twice the proportion of those with no long-term conditions.

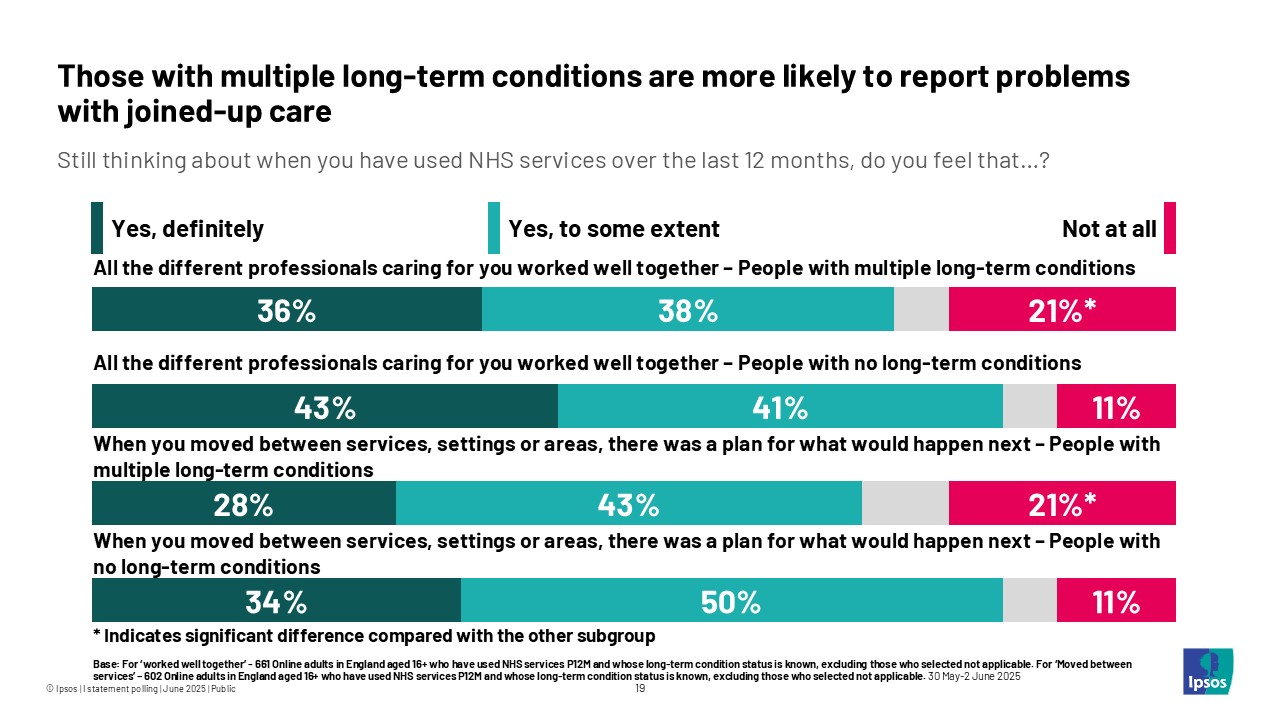
People with multiple long-term conditions are also more likely to require high quality, joined-up, integrated care to help manage their physical and mental health. Our research shows they are also more likely to report poor experiences here, compared with those who do not have any long-term conditions. One in five (21%) say that the different professionals caring for them did not work well together at all. The same proportion say there was no plan for what would happen next when they moved between services. This compares with one in ten (11%) of those with no long-term conditions.
What does this mean for the future?
We expect the 10 Year Plan to make some bold promises about patient power, about giving people more choice, control and agency over how they manage their own health. This will be driven in part through culture change of designing services around the convenience of patients not around providers, but also through the rapid adoption of new technology.
We also expect the Plan to put an increased emphasis on the outcomes the NHS is achieving, not just reporting how busy services are.
At the moment though, how progress against all this will be measured is not clear, and that’s a problem. In the NHS that old adage rings loud and true, what gets measures, gets done.
Our new research provides Government with a valuable baseline for understanding on public experiences of the NHS as it stands on the cusp of significant transformation. More importantly, it shows the potential of using 'I' Statements as a framework for measuring the success of the NHS and showing how Government is prioritising what matters most to people.
Using this baseline, National Voices will continue to advocate for 'I' Statements as way of understanding, and indeed driving, progress as the Government moves from the planning phase to implementation.
Technical note:
- For the full findings, click here.
- Ipsos surveyed a representative sample of 984 adults aged 16+ in England. Surveys were conducted online between 30 May and 2 June 2025. Data are weighted to match the profile of the population. All polls are subject to a wide range of potential sources of error.



