Improving access to healthcare by removing transportation barriers
Current, accurate, and actionable data is vital for transportation planners, policymakers, and healthcare providers to address transportation insecurity and its impact on healthcare access. Addressing social needs, like transportation issues, that arise when people try and access healthcare can improve quality of care outcomes and lower costs, particularly for underserved communities.[1],[2]
Nationally, about one in five Americans experienced some transportation-related barrier that prevented them from receiving medical care in the past year, according to a new nationally representative Ipsos poll.
This independent survey shows that these transportation barriers to healthcare access led to less frequent doctor visits and worsened overall healthcare outcomes, particularly among vulnerable populations, like those with lower income.[3]
Transportation agencies and healthcare providers must work together to understand and address this inequitable access to healthcare. Merging transportation and health data at the population and community level can provide powerful insights to inform policy and intervention strategies to make healthcare more accessible and equitable for patients and more cost-effective for the system overall.
This Ipsos data provides a preliminary glimpse at how transportation and health-related social needs data can be combined to provide deeper insights into transportation barriers to healthcare. Still, more data and standardized data practices can continue to help formulate a blueprint for decision-makers to tackle these barriers head-on.
Too much time and no public transit: The transportation barriers keeping people from healthcare
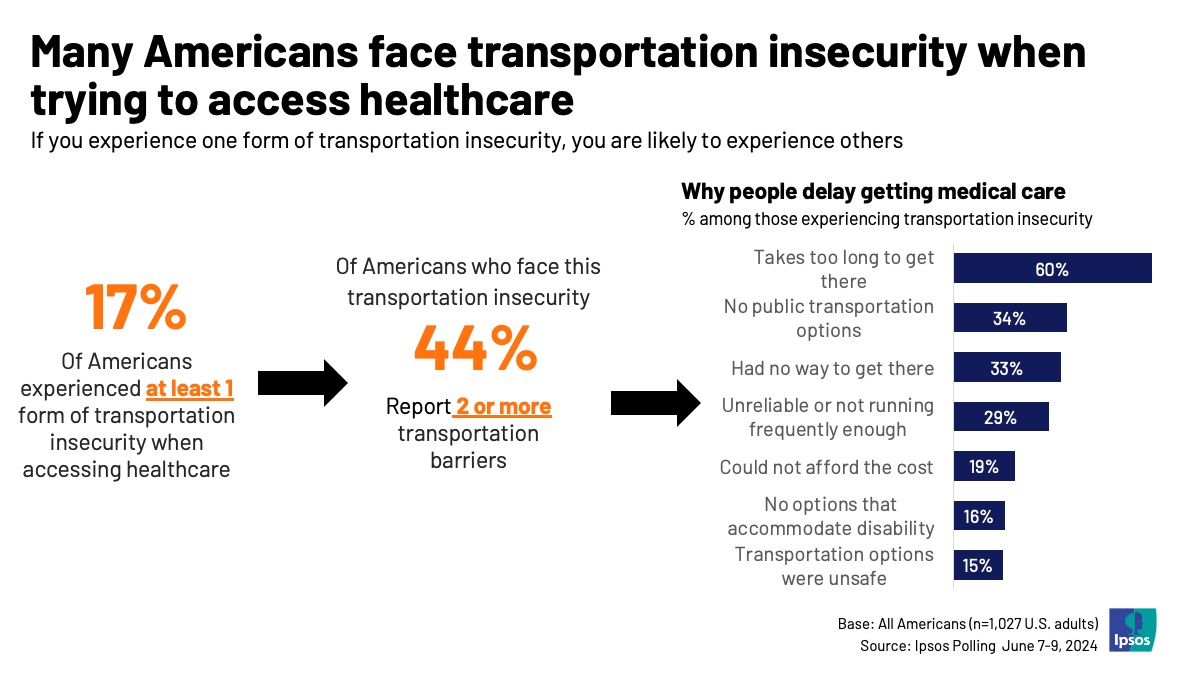
Overall, just under one in five Americans report experiencing some transportation barrier preventing them from accessing healthcare. Extrapolating that to the wider population, translates to roughly 67 million Americans who report difficulty accessing healthcare because of transportation barriers alone.
Among Americans who experienced a transportation-related barrier, the most common barriers involved include transportation taking too long to get to their appointment, having no public transportation options, no way to get to an appointment, or transportation being unreliable or not running frequently enough.
To that end, experiencing one transportation barrier to healthcare makes Americans more susceptible to experiencing multiple, highlighting the potentially compounding nature of the problem. Nearly half of Americans who experienced any form of transportation insecurity when trying to access healthcare also report experiencing two or more barriers.
These transportation barriers may affect healthcare outcomes. Those experiencing transportation insecurity are less likely to have seen a general doctor or dentist in the past year. They are also less likely to rate their overall health favorably.
Delaying or forgoing regular doctor’s appointments can be dangerous for patients and costly for healthcare systems. Research from the National Institute of Health suggests that patients using Medicare who did not regularly attend doctor’s appointments had more emergency department visits, more hospitalizations, and higher costs.[4] Being able to access healthcare is better for patient outcomes and is more cost-effective.
Who is most at risk of healthcare inequality?
Not every American experiences these issues equally. In particular, Hispanic, lower-income, younger, and less educated Americans are all more likely to report experiencing transportation barriers than the average American.
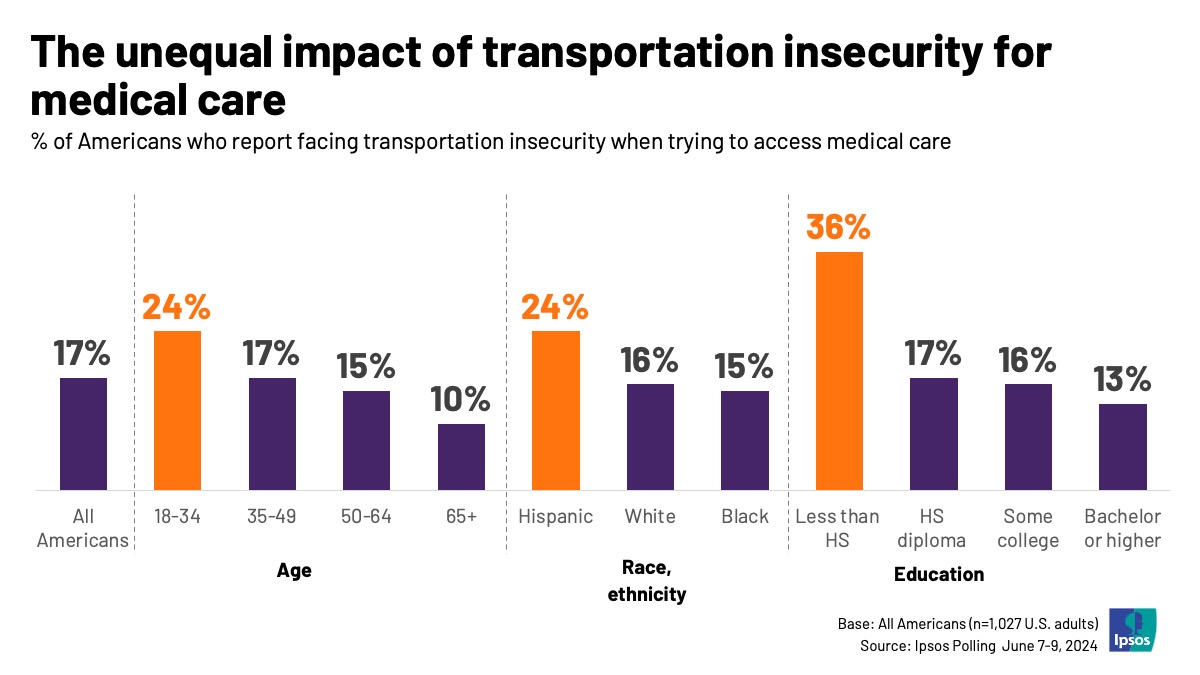
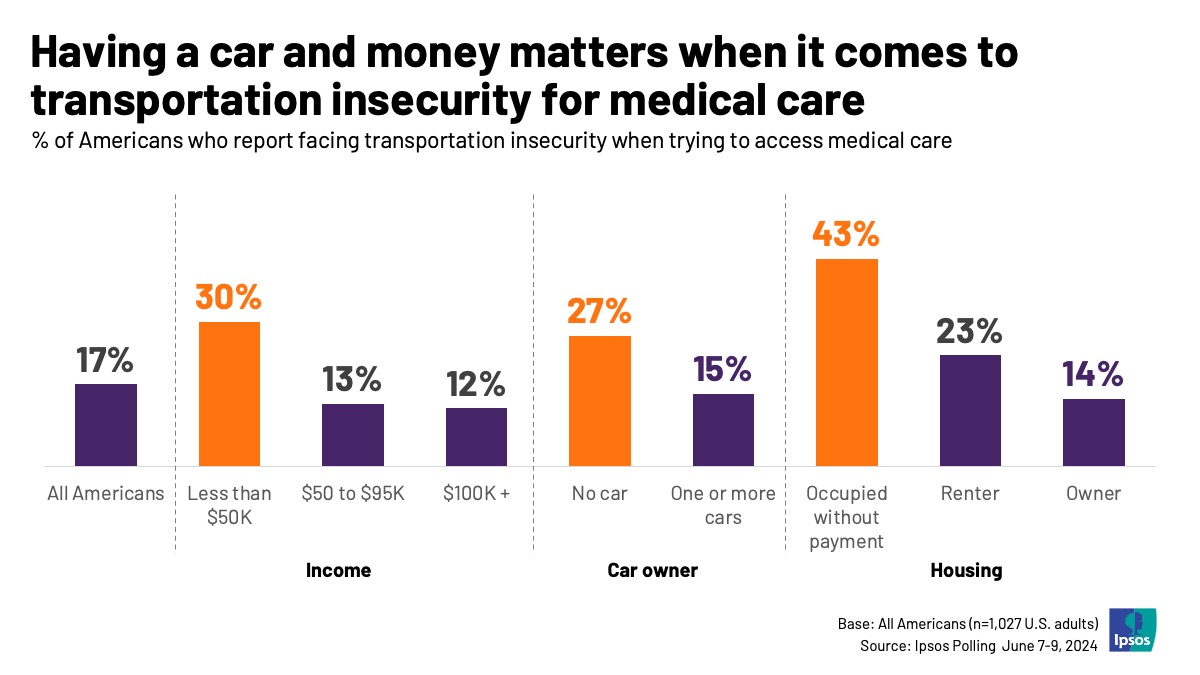
Transportation is a particularly important issue to address for low-income Americans. Americans with incomes under $50K are much more likely to say they could not afford transportation, that transportation was unreliable, or that there were no public transportation options available to them. Notably, Americans under 40 who also have incomes under $50K are among the most likely to experience these barriers, demonstrating how these issues can intersect.
Additionally, Americans who are behind on rent or mortgage payments are nearly as twice as likely as renters and three times as likely as homeowners to face transportation barriers to healthcare. Transportation barriers impact many marginalized groups, many of whom are already struggling.
Outside of these groups, non-car owners are two times more likely than car owners to experience barriers to healthcare access, reporting that it would take them too long to get to an appointment and that there were no public transportation options at higher rates. Car owners also experience transportation insecurity, just at lower rates than non-car owners.
Unreliable, overly lengthy, or unsafe transportation is also a health hazard. Ipsos data shows that Americans who experience these transportation barriers are less likely to visit their doctor’s appointments and less likely to rate their health favorably, particularly among vulnerable demographics.
Healthcare providers and transportation planners must work together to bridge these gaps in transportation access to create a more equitable and cost-effective healthcare system.
Ultimately, high-quality transportation data coupled with survey research that provides insights into the gaps and issues people face can give transportation planners, policymakers, and healthcare providers the insights needed to tackle these issues head-on.
This report exemplifies the power of research that addresses multiple societal challenges in tandem. By examining the impact of transportation barriers on healthcare access, the study not only highlights a critical issue but also demonstrates how an integrated approach—one that considers the intersections of transportation, healthcare, and social determinants of health—leads to more holistic, sustainable solutions. When we focus on the full range of obstacles that people face in their daily lives, such as transportation insecurity, we can better tackle social determinants that can be addressed to support better health outcomes. By looking at the whole picture of a person’s life, rather than only on a health condition, we can learn how to devise effective solutions to healthcare access. Addressing one issue in isolation often results in fragmented solutions, whereas considering multiple overlapping challenges allows program developers and policymakers to design interventions that are truly effective, equitable, and cost-efficient for the communities most in need.
—Elisa Borah, PhD, Director, Moritz Center for Societal Impact, Steve Hicks School of Social Work, UT Austin
What you can do
This research is just the tip of the iceberg for providers and transportation planners to bridge the health equity gap. The burgeoning need for connected digital health hold important implications for private companies too, as many work to create solutions in this space. Companies and agencies must learn to act smarter. Ipsos, through our gold standard probability-based KnowledgePanel, can run rigorous research to explore critical policy questions and identify where people are falling through the cracks. Some potential areas for future research include:
- Health Insurance and Compounding Inequality: How does health insurance status impact transportation barriers to healthcare, and how might that interact with socioeconomic status or other demographics?
- Impact of Transportation Insecurity on Healthcare Decisions: Are Americans in transportation deserts forgoing healthcare until their concerns are more serious and costly? Understanding how transportation insecurity influences healthcare decisions, such as delaying or forgoing care, choosing providers based on accessibility, and adhering to treatment plans may offer insights into low-cost interventions that can improve healthcare outcomes for vulnerable communities.
- Preferences for Transportation Solutions: Explore public preferences and awareness for different transportation or technology solutions that can help address healthcare access.
This sample covers the national population, but state and local authorities need to investigate at the state and local level to uncover nuances within the populations they serve. Solutions developed through innovative research at this local and state level are critical for identifying and addressing issues. Ipsos offers bespoke research services at these different levels so agencies can better meet and understand the needs of their constituencies and bridge the healthcare transportation equity gap.
Contact
For mobility-related research questions, reach out to:
Joann Lynch
Director, Public Affairs
[email protected]
For healthcare-related research questions, reach out to:
John Boerstler
Executive Vice President, Public Affairs
[email protected]
Zachary Lewis
Senior Vice President, Public Affairs
[email protected]
For questions about healthcare and the private sector, reach out to:
Chareen Lim
Senior Vice President, Healthcare
[email protected]
About Ipsos
At Ipsos, we are passionately curious about people, markets, brands, and society. We deliver information and analysis that makes our complex world easier and faster to navigate and inspires our clients to make smarter decisions. With a strong presence in 90 countries, Ipsos employs more than 18,000 people and conducts research programs in more than 100 countries. Founded in France in 1975, Ipsos is controlled and managed by research professionals.
[1] “CMS.” Accountable Health Communities Model Evaluation of 2018–2023, www.cms.gov/priorities/innovation/data-and-reports/2023/ahc-second-eval-rpt-fg. Accessed 18 Nov. 2024.
[2] “Social Drivers of Health and Health-Related Social Needs.” CMS.Gov, 21 Aug. 2024, www.cms.gov/priorities/innovation/key-concepts/social-drivers-health-and-health-related-social-needs#:~:text=The%20specific%20factors%20that%20impact,lack%20of%20access%20to%20transportation.
[3] This survey analyzes the recently established ICD-10-CM code for transportation insecurity developed by the World Health Organization and the National Center for Health Statistics. Social Determinants of Health (SDOH) Data with ICD-10- ..., www.cms.gov/files/document/cms-2023-omh-z-code-resource.pdf. Accessed 14 Nov. 2024.
[4] Rose, Adam J, et al. “Primary Care Visit Regularity and Patient Outcomes: An Observational Study.” Journal of General Internal Medicine, U.S. National Library of Medicine, 26 Oct. 2018, pmc.ncbi.nlm.nih.gov/articles/PMC6318173/#:~:text=Within%20each%20visit%20frequency%20group,more%20hospitalizations%2C%20and%20higher%20costs.

![[WEBINAR] Know America at 250: Public Opinion Update](/sites/default/files/styles/list_item_image/public/ct/news_and_polls/2026-02/250_0.png?itok=UwPuoNWi)

![[WEBINAR] Changing Focus: How 2026 will be different for global Influentials and Company Leaders](/sites/default/files/styles/list_item_image/public/ct/event/2026-02/thumbnail-0305-Influentials.jpg?itok=ZWeDU7Op)