The importance of communication and relationships with healthcare professionals for patients with mental health conditions: what does the NHS Adult Inpatient Survey tell us?
What is the Adult Inpatient Survey?
The Adult Inpatient Survey, commissioned by the Care Quality Commission (CQC), looks at the experiences of adults who have been an inpatient at an NHS hospital. The survey, published cross-sectionally on an annual basis, has been running since 2002. The survey also collects information about patients’ demographics (such as age, religion, ethnicity, long term conditions) in order to understand differences in care.
In total, 8% of the patients who responded to the 2021 survey reported that they have a mental health condition, disability or illness that has lasted or is expected to last 12 months or more. While this is a relatively small percentage, these patients represent an important group and it’s important to consider the aspects that may affect their care.
The importance of relationships and communication between healthcare professionals and patients
The relationship and trust between health care professionals and patients can often be complex and influenced by many different factors, such as communication, reassurance, respect, rapport and the way that patients perceive they are treated. However, these relationships are important as they help create an environment where patients are supported to accept their care and treatment plans, often leading to better health outcomes. This is particularly the case for the treatment of long-term illnesses, as well as supporting patients to make healthier lifestyle choices1,2.
On World Mental Health Day, it is important for us to consider how these relationships may differ for patients with mental health conditions. This is particularly important when we consider that people with mental health conditions can often have poorer health outcomes3.
The findings from the Adult Inpatient Survey 2021 show that while relationship with health care professionals and communication was generally to a high standard, patients with mental health conditions were generally less positive about their experiences than patients without mental health conditions.
Dignity and respect
Dignity and respect are at the core of how all of us would like to live our lives and is at the heart of healthcare regulation4. While the majority of patients with mental health conditions felt they were treated with respect and dignity during their hospital stay, the proportion reporting they were always treated this way was significantly lower than patients without mental health conditions (68% vs 83%).
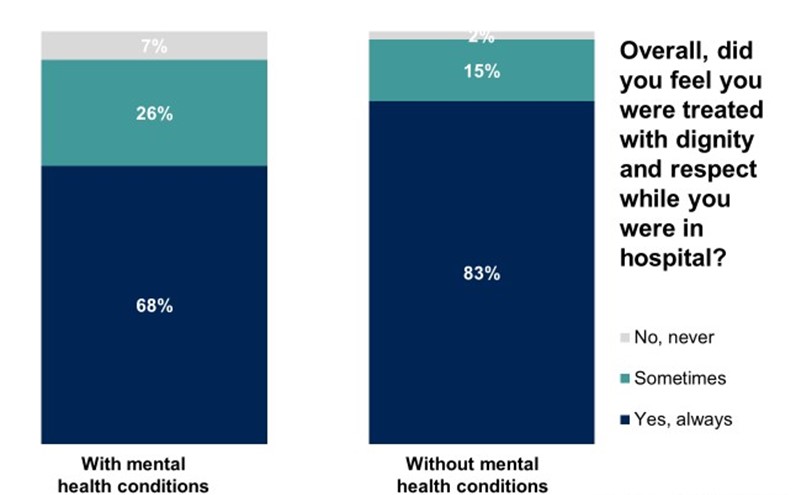
Base (weighted): All inpatients who participated in the Adult Inpatient Survey: with mental health conditions (5,592), without mental health conditions (53,921).
Confidence and trust in health care professionals
Although confidence and trust in health care professionals were generally high, patients with mental health conditions were significantly less likely to report they trusted them compared with patients without mental health conditions. For example, 67% of patients with mental health conditions reported they always had confidence and trust in their doctors, compared with 83% without. A similar pattern was found for nurses, with 69% reporting they always had confidence and trust, compared with 80% of patients without mental health conditions.
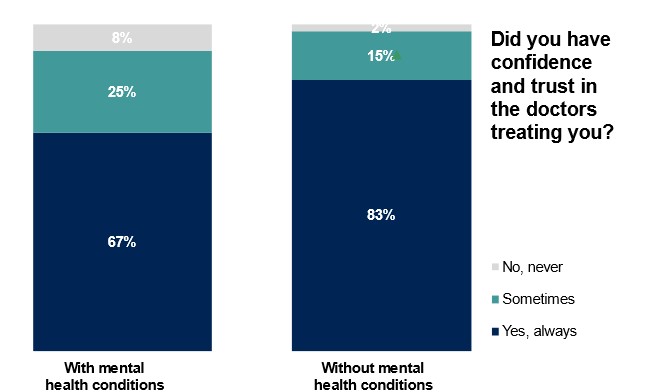
Base (weighted): All inpatients who participated in the Adult Inpatient Survey: with mental health conditions (5,578), without mental health conditions (53,759).

Base (weighted): All inpatients who participated in the Adult Inpatient Survey: with mental health conditions (5,577), without mental health conditions (53,757).
Consistency of information provided
Consistency of information received from healthcare professionals is a key area that affects how patients view their care. Patients with mental health conditions were more likely to report they had been told different information by different members of staff compared with patients without a mental health condition (54% yes always/sometimes compared with 35%).
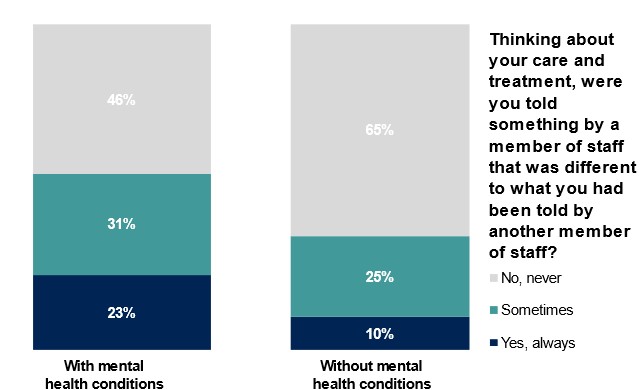
Base (weighted): All inpatients who participated in the Adult Inpatient Survey: with mental health conditions (4,937), without mental health conditions (48,086).
Reassurance
Across all measures we examine in this blog, being able to talk about their worries and fears with a member of staff during their hospital stay (reassurance) was reported the least favourably for patients with and without mental health conditions alike. Less than half of patients with mental health conditions (47%) reported they always felt able to talk to members of hospital staff about their worries and fears, compared with 61% of patients without mental health conditions.
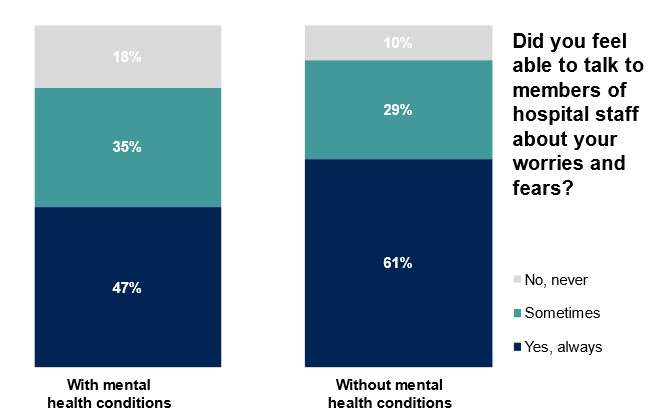
Base (weighted): All inpatients who participated in the Adult Inpatient Survey: with mental health conditions (5,203), without mental health conditions (44,940).
Conclusion
The rate of adults reporting clinical levels of mental health conditions has increased since 20195 and is estimated to occur in 16% of the UK population6. With evidence of inequalities in health care7, reduced life expectancy8, and increased risk of multimorbidity9, accessing quality health care, for people with mental health conditions, is of primary importance.
The Adult Inpatient Survey 2021 shows health care professionals have developed relationships, and ensured positive communication styles, with patients with and without mental health conditions. Yet patients with mental health conditions consistently report poorer relationships with health care professionals and poorer communication during their hospital stay, showing that more needs to be done.
For the Care Quality Commission, NHS trusts, and stakeholders (such as NHS England and Health Watch England) communication and the patient-health care relationship is at the forefront of a successful patient journey. Strides have been taken throughout 2022 by all parties to promote quality care10,11. Future year on year comparisons of communication and the patient-health care professional relationship can explore whether this gap between patients with and without mental health conditions is reducing.
More information can be found on the Ipsos website and the CQC website.
Technical note
- Ipsos coordinates the Adult Inpatient Survey on behalf of the CQC. NHS trusts selected a sample of 1,250 patients, aged 16 or over, who had stayed at least one night in hospital during November 2021. The survey was conducted using a mixed methods approach, combining online and paper questionnaire modes. A total of 62,235 patients responded to the survey (an adjusted response rate of 39%) and fieldwork took place between January 2022 and May 2022.
- The subgroup analysis referred to in this blog compares how different groups of patients, with and without mental health conditions, rated their overall experiences of being a hospital inpatient. Responses to questions relating to relationships and communication between healthcare professionals and patients have been weighted, whereas grouping of patients (with or without mental health condition) remains unweighted. More information on this analysis and the questions included can be found on the NHS Surveys website: https://nhssurveys.org/
- Results for the Adult Inpatient 2021 Survey are comparable with results from 2020, but not with results from years prior to 2020 due to a change in survey methodology.
- Further technical information and the full survey results can be found on the CQC website.