What does the NHS Maternity Survey 2022 tell us about maternity services since the pandemic?
What is the Maternity Survey?
The Maternity Survey, commissioned by the Care Quality Commission (CQC), started in 2007 and the 2022 survey is the ninth to be carried out. It looks at the experiences of women and other people that gave birth at an NHS Trust in England. The survey also collects information about demographics (including characteristics protected by the Equality Act 2010, such as age, long-term condition, religion, and ethnicity), in order to understand differences in experience of care.
What has changed in the past year?
Results from the survey show some changes in experiences of maternity services compared with previous years. Across the survey there are twenty-six questions which show five-year trends between 2017 and 2022. Out of the twenty-six questions, twenty-one show a downward trend with this year being the lowest point for ten questions. Areas of decline include:
- Staff availability: Across the maternity pathway there has been a decline in the proportion of respondents who say they can always get help when they need it. For example, 69% stated that they were always given the help they needed during their pregnancy when they contacted the midwifery team. This is down from 75% in 2019 and 70% in 2021. Similarly, 63% of women and other people giving birth reported that during labour and birth they were always able to get a member of staff to help them when they needed it. Again, this shows a fall on previous years (72% in 2019, and 65% in 2021).
Similarly, when asked if they (or their partner/companion) were left alone by midwives or doctors at a time when it worried them, there is a decline in those who say ‘no’ from 78% in 2019 to 74% in 2022. - Information and advice: Related to the availability of staff, the provision of information and advice has also dropped. While most (82%) respondents felt they were given appropriate advice and support at the start of their labour, this is a drop from 88% in 2019 and 84% in 2021. Overall, 59% of women and people who had given birth said yes, they were always given the information or explanations they needed in hospital after the birth of their baby, but again this represents a decrease in the provision of information (66% in 2019 and 61% in 2021).
- Interactions with staff: Almost a quarter of women and people who had given birth (23%) felt that when they raised a concern during labour and birth, it was not taken seriously, representing an increase over time (from 16% in 2019 and 21% in 2021).
The proportion of respondents who stated they had confidence and trust in the staff caring for them has declined over time; 78% in 2022, compared with 80% in 2021 and 84% in 2019. This is mirrored by a drop in the proportion who feel that they were always treated with kindness and understanding (71% in 2022, down from 76% in 2019). - Midwifery continuity of carer: The Better Births maternity review recommends that there is continuity of carer throughout pregnancy, birth, and postnatally. Every woman and pregnant person should have a midwife who is part of a small team who can provide continuity throughout the pregnancy, birth, and postnatally. Continuity of carer remains a key variable when looking at the differences in experiences of maternity care. It allows for a build-up of trust and better understanding of the patient’s medical and pregnancy history, leading to better outcomes. However, only 37% of respondents saw or spoke to the same midwife at their antenatal check-ups, falling to 27% during postnatal appointments. This represents a decline in midwifery continuity of carer since 2021 but is in line with the findings from the 2019 Maternity Survey.
- Parity: Those who had given birth before reported better experiences of maternity care than those giving birth for the first time. This may be related to a limited availability of information: Only half of women and pregnant people stated that they were provided with relevant information about feeding their baby during pregnancy (53%, down from 57% in 2019), and two-thirds (64%) were always given support and encouragement about feeding their baby after birth (down from 69% in 2019). Around one in five (16%) also reported not being given information about their own physical recovery after birth (up from 10% in 2019).
Areas of improvement
There are some areas of care that have seen an upward trend across the years. One of these is the experience of discharge from hospital, where around two-thirds of women and other people who had given birth report no delay to their discharge (62%, up from 56% in 2019).
Additionally, the results show an improved experience around support for mental health across the maternity pathway.
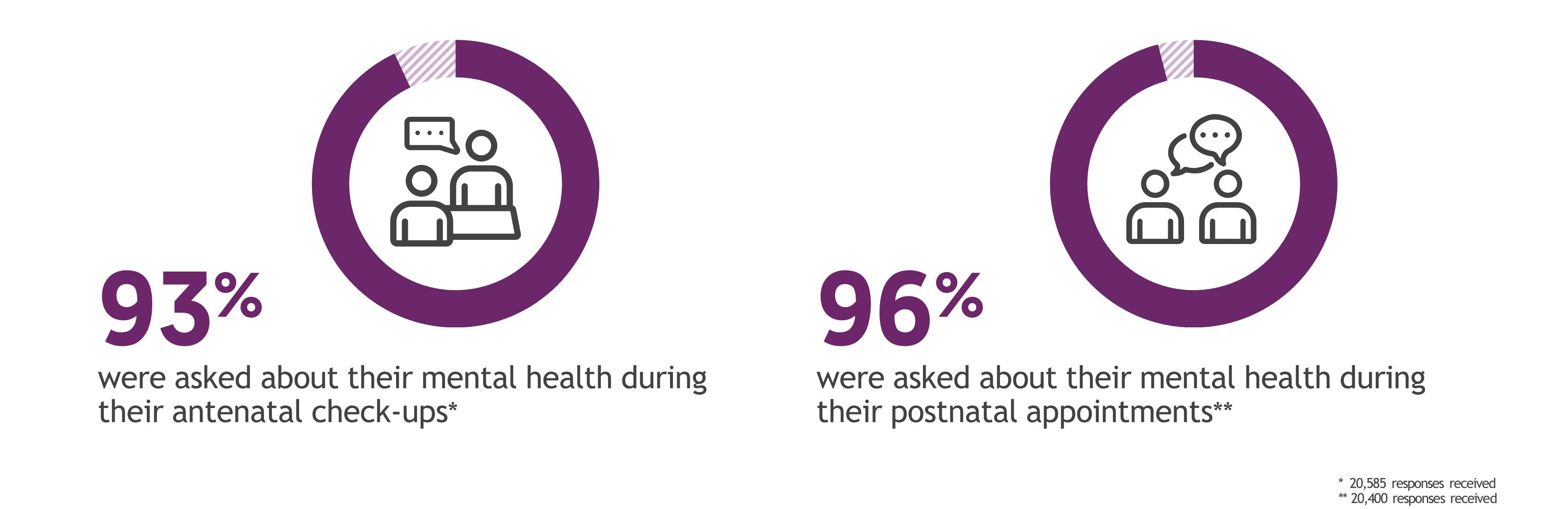
Nearly all women and other people who had given birth report that they were asked about their mental health during antenatal check-ups; 96% stated that their midwife or health visitor asked them about their mental health (up from 95% in 2021). Most women and other pregnant people (85%) also say they were given enough support for their mental health during their pregnancy (up from 83% in 2021).
I received care from an enhanced midwife and perinatal mental health team due to a mental health problem identified in my last pregnancy. This team was absolutely fantastic – particularly my enhanced midwife, obstetrician, psychologist, psychiatrist, and nurse. The care they provided was outstanding. I felt very supported throughout my pregnancy – could not have done it without them!
Continued impact of COVID-19
In February 2022, coronavirus restrictions continued to have an impact on maternity care. Out of the twenty-six trend questions, eighteen declined during the pandemic, as shown by the 2021 Maternity Survey results. Out of those, five have seen further decline this year, and six have stayed at the same level, suggesting that the impact of the pandemic on maternity services has continued.
One area of the maternity journey that has continued to suffer due to the pandemic is the involvement of birthing partners. Two in five (42%) said there were some coronavirus restrictions in place that affected how involved their partner could be. While this is down from 66% in 2021, it remains high.
The proportion of respondents saying their partner could be involved as much as they wanted during labour and birth has recovered slightly (90% in 2022 vs 84% in 2021) but remains below pre-pandemic levels (97% in 2019). The recovery has been slowest in postnatal care on the ward, with less than half (41%) reporting that their partner was able to stay with them as much as they wanted during their stay in hospital, compared to pre-pandemic levels of 74% (34% in 2021).
I hated not having my husband present in triage and for antenatal appointments. I think it was extremely unfair and does not value the importance partners play in pregnancy, labour, and postnatal support.
Overall, these results are in line with other national patient experience surveys, such as the NHS Inpatients Survey which showed a significant decline in staff availability, support given by staff to meet fundamental needs, and waiting times. The GP Patient Survey also reported decreases in overall experience of GP practices, the process of making GP appointments, and NHS services when the GP practice is closed. The national picture also no longer seems to reflect the ‘gratitude bias’ that was evident during the pandemic, with latest polling data showing that around half (55%) think the general standard of NHS care has gotten worse in the last year, and around a third think the NHS is not providing a good service nationally (35%) or locally (33%).
Conclusion
This survey provides invaluable insight into the post-pandemic experience of maternity services and adds to the national picture of care currently characterised by concern and pessimism among the public and service users and reflects the significant strain the NHS is operating under. Despite these difficulties, there is still strong support from the public for the NHS, with 77% of the UK public believing it is ‘crucial to British society and we must do everything to maintain it’. This survey and other surveys that measure people’s experiences of care are vital for NHS Trusts to understand how they can improve their services to ensure all patients receive safe, effective, and compassionate care.
More information can be found on the NHS Surveys website and the CQC website.
Technical note
- Ipsos coordinates the Maternity Survey on behalf of the CQC. NHS Trusts draw a sample of all patients, aged 16 or over, who had given birth during February 2022. If there were fewer than 300 maternity service users within an NHS trust who gave birth in February 2022, then births from January were included.
- The survey was conducted using a mixed methods approach, combining online and paper questionnaire modes. A total of 20,927 patients responded to the survey (an adjusted response rate of 46.5%) and fieldwork took place between April 2022 and August 2022.
- Results for the Maternity Survey 2022 are comparable with results from 2013, 2015, 2017, 2018, 2019, and 2021, but not with results from years prior to 2013 due to a change in survey methodology.
- Further technical information and the full survey results can be found on the CQC website.






