NHS 75: How behavioural science can unlock the potential of digital health
There is no denying that the NHS faces unprecedented challenges. With its capacity to meet demand for services under extreme pressure, digital innovations offer hope of reducing unnecessary demand and maximising its efficiency, through tools such as virtual wards and remote monitoring. This blog considers how behavioural science can support the adoption of digital health interventions, which will be an important component of the NHS’ future.
Public and professionals call for digital health interventions
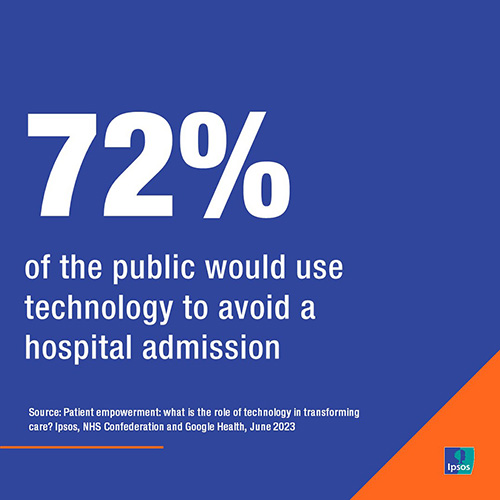
There is an appetite amongst the public for self-management of their care using digital health interventions. Ipsos research for the NHS Confederation and Google Health into the role of technology in transforming care and patient empowerment found that:
- More than 7 out of 10 (72%) would use technology to avoid a hospital admission, and this was true across all age groups.
- More than 7 in 10 people (72%) would also use technology including wearable and health monitoring devices to help better manage and monitor their health and would be willing to share the information and data gathered with their doctors and other medical professionals.
- Nearly 4 in 5 people (78%) would be happy to use different types of health monitoring equipment to help manage their health if an NHS professional recommended it to them, with nearly 9 in 10 (89%) people aged over 75 willing to do so.
Alongside public appetite for technology in health, there is also significant support from physicians to increase the use of digital health interventions.
Ipsos’ Digital Doctor Health Tracker Survey research found that:
- 71% of physicians say in home self-monitoring tools are the future of healthcare.
- 84% of physicians think connected health devices for patients will form part of treatment plans for certain health conditions in the future.

This isn’t to say physicians are without concerns about the potential increase in digital health interventions such as wearables and health monitoring devices.
- Over half of physicians surveyed say patients may misinterpret data (58%) or self-diagnose/ self-manage without physician supervision (52%).
That being said, our survey showed an understanding amongst physicians that these technologies will become an increasingly important part of patient care in the future. So despite clear support from both patients and physicians for digital health interventions, it might be surprising to see that uptake is relatively low.
Ipsos’ paper on The Unrealised potential of digital therapeutics in the UK showed:
- 54% of the UK public have never used technologies to monitor their health.
- 92% have never used a treatment that could be considered a Digital Therapeutic (DTx) (defined as evidence-based, software-driven therapeutic interventions such as online tools, communities and apps).
This gap between support for digital health interventions and current usage indicates a significant opportunity area for the NHS; one where behavioural science can play a pivotal role in increasing uptake.
How behavioural science can boost uptake
So what can behavioural science tell us about increasing the uptake of digital health interventions such as wearables and health monitoring devices?
Behavioural science can offer us a structured way of understanding why uptake of digital health interventions is relatively low at present and how engagement can be boosted.
Using the COM-B model for behaviour change, a recent systematic review identified 26 key factors across the constructs of ‘capability’, ‘opportunity’ and ‘motivation’ that influence the uptake of and engagement with health and wellbeing apps.
Recommendations for increasing engagement with health and wellbeing apps focused around:
- Increasing awareness
- Improving app literacy skills
- Providing web-based or offline health practitioner support
- Providing endorsement from healthcare professionals
- Positive feedback, rewards and goal setting
In a recent behavioural study by Ipsos looking at the uptake of a digital weight management programme, many of these factors were also observed as being key to increasing engagement, alongside the provision of personalised support that was tailored to individuals’ particular situations and goals, and the authenticity of NHS branding as a trusted body. Behavioural studies such as these therefore have implications for policy makers, industry and healthcare providers who wish to see greater uptake of digital health interventions among the public.
As we look to the future of the NHS, digital innovation offers us opportunities to better manage and monitor our own health. What we must be mindful of is the risk of digital exclusion, with these developments benefitting some but not all. Using behavioural science to understand issues of digital access, inclusion and confidence could be key to ensuring a more universal uptake of digital health interventions and the patient empowerment that they can bring.