Maternal mental health support continues to improve despite NHS strain
Statistics show that one in five women develop a mental health problem during pregnancy or within a year of giving birth1. In the last 12 months alone, more than 45,000 women accessed specialist community perinatal mental health services2, making it a crucial part of maternity care.
When it comes to maternal mental health, the UK has come a long way in the last decade. In 2014, less than 15% of localities provided specialist services for women with complex or severe perinatal mental health conditions3. In 2016, Better Births4, a national maternity review, called for better postnatal and perinatal mental health care, asking for better investment and appropriate resourcing. This came at the same time as a government announcement of a £290m investment into new specialist perinatal mental health services5. The investment, paired with renewed visibility of maternal mental health as a priority, led to these services being available in every locality across England6 since 2019.
The majority of women feel supported, according to the NHS Maternity Survey
Whilst the results of the 2022 NHS Maternity Survey7 showed general downward trends8, mental health support was among the few measures displaying improvement, with 85% of respondents reporting that they were given enough support for their mental health during their pregnancy, up from 83% in 2021.
Figure 1. Percentage of respondents reporting they were given enough support for their mental health during their pregnancy.
This is an achievement considering the current context of maternity care, with the perceived availability of staff having deteriorated at every stage of the maternity care as shown in figure 2.
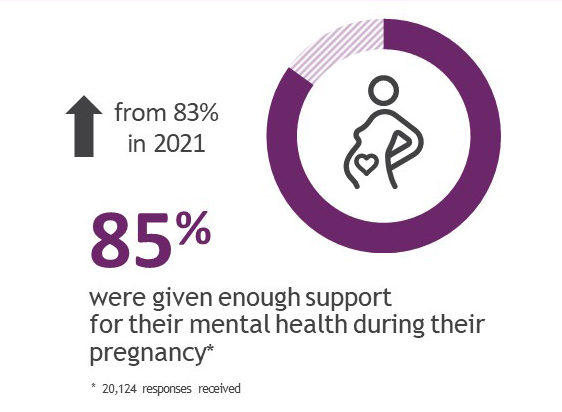
Figure 2. Perceived availability of staff at every stage of maternity care.
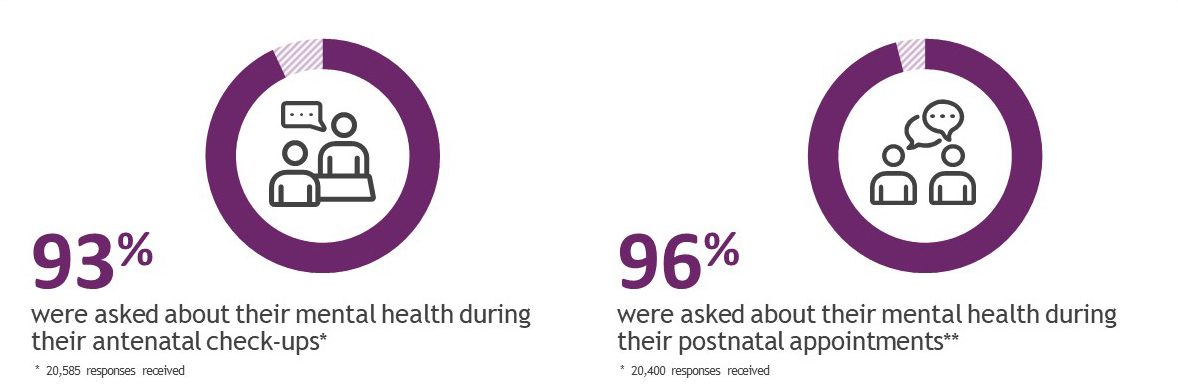
Additionally, more than nine in ten respondents report that they were asked about their mental health during their antenatal check-ups (93%) and postnatal check-ups (96%).
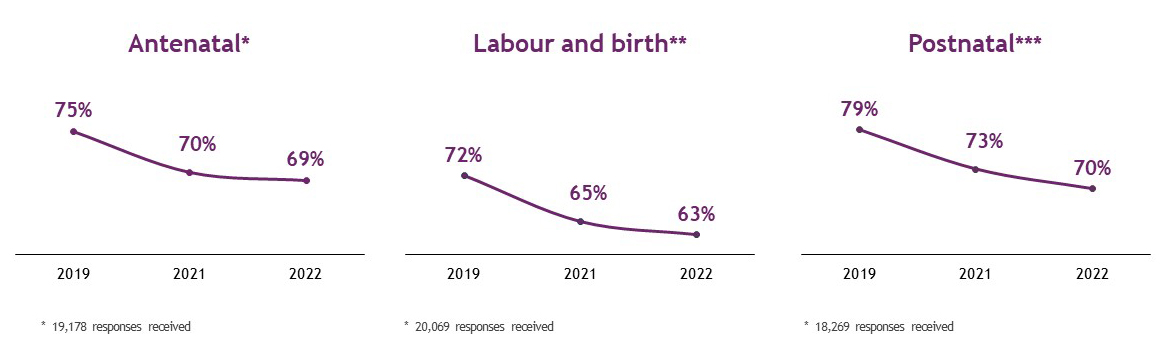
Figure 3. Percentage of respondents reporting they were asked support for their mental health during their pregnancy.
The above figures are supported by comments received from the respondents, detailing their personal journey and help they received.
Maternity Service User, 38, North East
My health visitor has been absolutely amazing. Around 4 weeks after the birth of my baby my mental heath deteriorated due to a health concern. She helped and offered advice on said health concern and was extremely supportive and came for extra visits. When I had the all clear I was unable to come out of the depression I had fallen into and she directed me to the perinatal mental health team. She is still a support to me now and I honestly don't know what I would have done without her.
Improvement is needed in postnatal care
The 2022 NHS Maternity Survey data shows that even though mothers’ mental health is supported whilst under hospital care, the support drops off after being discharged. One in five respondents indicated that they were not told who to contact if they needed advice about changes they might experience to their mental health after birth.
The 6-week postnatal check-up with the GP in particular emerged as a weak point in maternal mental health support, where almost a third (29%) said that the GP did not spend enough time talking to them about their own mental health during the check-up.
Maternity Service User, 31, East of England
My 6 week post natal check was done over the phone (at 8 weeks) . Not once was I asked about my mental health which I felt was not good enough, especially considering I had a difficult labour and suffered a third degree tear.
Lastly, the lack of continuity of carer which was highlighted as a priority in the original 2016 Better Births report, and again in the 2020 progress report9 could be contributing to worse mental health amongst service users. The NHS Long Term Plan10 set out in January 2019 called for 75% of Black, Asian, and ethnic minority service users, and those from the most deprived areas to be provided with continuity of carer11 by March 2024. Whilst not directly linked to mental health support, it supports building trust between the midwife and the service user, and facilitates better support for those who may struggle to ask for it.
Maternity Service User, 32, Midlands
I would add that there does need to be a bigger focus on postnatal support, especially mental health as I did struggle after the initial sigh off period. Though it may not be possible, it would be beneficial to have consistent midwife throughout antenatal and postnatal care to build a better rapport to seek confidence in asking for help of needed.
It is important to continue to track maternal mental health experience
The NHS Maternity Survey demonstrates that in England maternal mental health services are generally doing well, with more than nine in ten mothers reporting being asked about their mental health both antenatally and postnatally. However, some parts of postnatal support are lacking - a small but important proportion of mothers is not being told who to contact if they need advice about postnatal mental health. Additionally, the GP check ups which were introduced to focus on the mother’s physical and mental health are not always delivering on the promise, with a third of service users reporting that the GP did not spend enough time talking to them about mental health at the 6-week check-up.
Mental health problems are the leading cause of death in pregnancy and the 12 months after birth12, and whilst the above results are encouraging, they also show that there is still some way to go for maternal mental health services. It will be important to continue to monitor the support and other factors that play into mothers’ mental wellbeing and safety.
Technical Note
- The NHS Maternity Survey is designed to capture the views of individuals across the maternity pathway, providing important insights into their experiences and the quality of the care they receive. It’s been running since 2007, and 2022 marked its ninth iteration.
- Ipsos coordinates the Maternity Survey on behalf of the Care Quality Commission (CQC). NHS trusts drew a sample of mothers, aged 16 or over at the time of delivery, and had a live birth between 1 February and 28 February 2022. If there were fewer than 300 mothers within an NHS trust who gave birth in February 2022, then births from January were included.
- 45,621 mothers were invited to take part in the survey and 20,927 mothers responded (an adjusted response rate of 46.5%).
- Fieldwork took place between April 2022 and August 2022.
- Ipsos is coordinating the 2023 Maternity Survey on behalf of CQC, which will be running between May and August 2023.
- Prior to 2021, the Maternity Survey was conducted using a solely paper-based methodology. Following a successful pilot of a mixed method approach, the 2021 survey transitioned to offer both paper and online completion methods. You can view this work on the cross survey programme website.
- Further technical information and the full survey results can be found on the CQC website



